CASE REPORT
A Hydatidiform Mole Can Cause Severe Gestational Hyperthyroidism
Shalini Bhat and Jelena Maletkovic*
Clinical Thyroidology
OBJECTIVE: To report a new case of molar pregnancy associated with severe thyrotoxicosis.
Background
Gestational trophoblastic disease (GTD) is a rare complication of pregnancy that may be associated with thyrotoxicosis. The incidence of hydatidiform mole in the United States and other developed countries is about 1 in 1500 live births (1). Complete moles have the highest incidence of thyrotoxicosis, predominantly affect younger women, and present with vaginal bleeding most of the time. Hyperthyroidism in hyperemesis gravidarum occurs with greater frequency than in normal pregnancy. We describe a case of hyperthyroidism secondary to molar pregnancy highlighting the rare but important evaluation of hyperthyroidism in women of child-bearing age.
Case Report
A 20-year-old woman, gravida 2, para 1, presented to the emergency room with a history of nausea, weight loss of about 20 lb in 6 weeks, and intermittent vaginal bleeding. On examination, she had tachycardia (108 BPM), a blood pressure of 146/86 mm Hg, and a regular respiration rate of 18 breaths per minute. There was no exophthalmos, and her extraocular movements were normal. The thyroid gland was palpable and of normal size. Cardiovascular examination revealed sinus tachycardia without murmurs, rub, or gallops. Breath sounds were equal bilaterally, without rhonchi or wheezes. There was no peripheral edema. The size of the uterus was compatible with a 12-week gestation.
Ultrasonography of her enlarged uterus revealed that the uterine cavity was significantly distended and filled with an echogenic soft-tissue mass that had small cystic components, most compatible with complete molar pregnancy. Her thyroid-function tests were found to be markedly elevated (Table 1). Her thyrotropin (TSH) was <0.07 mIU/ml (normal range, 0.3 to 4.2), free thyroxine (FT4) 5.59 ng/dl (normal range, 0.8 to 2.0), triiodothyronine (T3) 465 ng/dl (normal range, 40 to 180), and human chorionic gonadotropin (hCG) close to 2 million mIU/ml. Laboratory data on admission revealed microcytic hypochromic anemia and elevated transaminase and alkaline phosphatase. The remainder of her electrolytes, complete blood count, and platelets were normal. Her electrocardiogram showed sinus tachycardia.
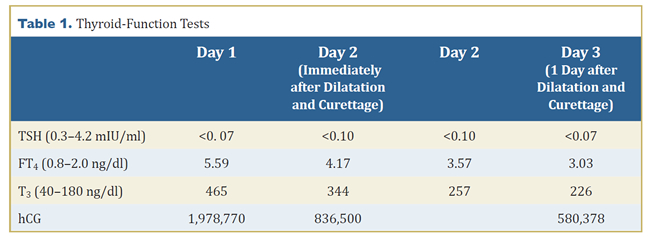
The patient underwent dilatation and curettage for evacuation of the mole. During the postoperative period respiratory failure secondary to noncardiogenic pulmonary edema developed. She required intubation and had a prolonged hospitalization but then stabilized and was discharged in good condition. Histopathology of all aborted specimens verified the diagnosis of partial mole, including a dystrophic fetus. The hCG values decreased to below detection after 12 weeks, and she was euthyroid at follow up with free T4 of 1.1 ng/dl and TSH of 1.42 mU/l.
DISCUSSION AND CONCLUSIONS • • • • • •
GTD with thyrotoxicosis is a rare clinical scenario, but thyroid hyperstimulation by hCG can have severe clinical consequences. Complete hydatidiform mole most commonly presents with vaginal bleeding, occurring at 6 to 16 weeks of gestation in 80% to 90% of cases (1). The clinical signs and symptoms, such as hyperemesis, have occurred less frequently in more recent years because of earlier diagnosis resulting from widespread use of ultrasonography and accurate tests for hCG. In the past, approximately 55% to 60% of women with trophoblastic disease had clinically evident hyperthyroidism that could be severe at the time of diagnosis. However, in a review of 196 patients from the United Kingdom treated for gestational trophoblastic disease between 2005 and 2010, biochemical hyperthyroidism was present in 7% and clinical hyperthyroidism in only 2% (2). Hydatidiform moles are commonly associated with hCG levels markedly elevated above those of normal pregnancy, as can be seen in our patient, who had an hCG level close to 2 million mIU/ml. Approximately 50% of patients with molar pregnancy have preevacuation hCG levels >100,000 mIU/ml (3).
Tisne et al. reported the first case of clinical hyperthyroidism in a patient with hydatidiform mole in 1955 (4). The glycoprotein hormone hCG is a specific tumor marker for trophoblastic diseases. The analogy in the structure between hCG and TSH can cause cross-reactivity with their receptors. It has been shown that the homology in the hCG and TSH molecules, as well as in their receptors, is likely to be responsible for the cross-reactivity of hCG with the TSH receptor (5). Glinoer has estimated that ”for every 10,000 mU/mL increase in serum hCG, FT4 increases by 0.1 ng/dL and TSH decreases by 0.1 mIU/mL” (6). Molecular variants of hCG found in molar pregnancies have increased thyrotropic potency (7). When gestational trophoblastic disease causes a significant rise in hCG levels, it may induce hyperthyroidism that requires treatment. As expected, thyrotoxicosis resolves with treatment of GTD and normalization of hCG levels. The development of hyperthyroidism is largely influenced by the level of hCG and usually resolves with treatment of GTD. The consideration of this cause of hyperthyroidism in pregnancy should be diagnosed early and managed efficaciously before imminent dilatation and curettage is required for definitive management of the hydatidiform mole.
*Endocrinology Division, UCLA School of Medicine, Los Angeles, CA
References
- Lurain JR. Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol 2010;203:531-9. Epub August 21, 2010.
- Garner E, Goldstein DP, Feltmate CM, Berkowitz RS. Gestational trophoblastic disease. Clin Obstet Gynecol 2007;50:112-22.
- Menczer J, Modan M, Serr DM. Prospective follow-up of patients with hydatidiform mole. Obstet Gynecol 1980;55:346-9.
- Tisne L, Barzelatto J, Stevenson C. Study of thyroid function during pregnancy-puerperal state with radioactive iodine. Bol Soc Chil Obstet Ginecol 1955;20:246-51. [in Spanish]
- Yoshimura M, Hershman JM. Thyrotropic action of human chorionic gonadotropin. Thyroid 1995;5:425-34.
- Glinoer D. The regulation of thyroid function in pregnancy: pathways of endocrine adaptation from physiology to pathology. Endocr Rev 1997;18:404-33.
- Pekary AE, Jackson IM, Goodwin TM, Pang XP, Hein MD, Hershman JM. Increased in vitro thyrotropic activity of partially sialated human chorionic gonadotropin extracted from hydatidiform moles of patients with hyperthyroidism. J Clin Endocrinol Metab 1993;76:70-4.
CLINICAL THYROIDOLOGY • DECEMBER 2013 VOLUME 25 • ISSUE 12 • © 2013



