
CLINICAL THYROIDOLOGY FOR PATIENTS
A publication of the American Thyroid Association
Summaries for Patients from Clinical Thyroidology by Ernest Mazzaferri, MD MACP
Table of Contents | PDF File for Saving and Printing
THYROID CANCER
What is the study about?
Papillary thyroid cancer (PTC) recurs in up to 30% of patients. Surgery and radioactive iodine therapy are the mainstays of therapy in such cases. The current ATA treatment guidelines recommend compartment-directed neck surgery for patients with lymph node metastases and no evidence of distant metastases (lung or bone) as the first line of therapy. The likelihood of repeat surgical interventions in rendering patients free of disease is currently unknown. The aim of this retrospective study was to determine the efficacy and safety of central or lateral neck lymph node dissection in patients with recurrent PTC.
The full article title: Schuff, K. G., Weber, S. M., Givi, B., Samuels, M. H., Andersen, P. E., and Cohen, J. I. Efficacy of nodal dissection for treatment of persistent/recurrent papillary thyroid cancer. Laryngoscope 118(5), 768-775. 2008. http://www.ncbi.nlm.nih.gov/
pubmed/18197134?dopt=Citation
Who was studied?
The study subjects were 75 patients who had 79 lymph node dissections for persistent/residual papillary thyroid carcinoma.
How was the study done?
The primary outcome was the thyroglobulin (Tg) response to lymph node dissection. The secondary outcomes were surgical complications.
What were the results of the study?
Of the 39 classifiable resections, 16 (41%) resulted in undetectable postoperative TSH-stimulated Tg levels. An additional 12 resections resulted in significant (50% or more) reductions in suppressed or TSH- stimulated Tg levels for an overall improvement rate of 72%. Of all 79 resections, 25 (32%) resulted in minor and 7 (9%) resulted in major complications. The 7 (9%) major complications, included permanent hypoparathyroidism (7% of resections at risk), significant abscess requiring tracheostomy for airway and management and operative drainage, and pulmonary embolism after deep venous thrombosis LND for persistent/recurrent PTC is a relatively safe procedure in experienced hands. It can lead to an undetectable Tg in 41% of cases and produce a major Tg reduction in an additional 31%.
What was the aim of the study?
This study was done to evaluate the efficacy and morbidity of lymph node dissection in recurrent/persistent papillary thyroid short-term follow-up is comparable with that reported for I-131, and it should be considered in the management of persistent/recurrent PTC.
How does this compare with other studies?
The data in this study, as well as some previous reports, suggest that in experienced hands, central compartment dissection does not increase the risk of hypoparathyroidism compared with lateral nodal dissection
What are the implications of this study?
In experienced hands, systematic compartment-based nodal dissection is a safe and efficacious treatment for persistent/recurrent PTC.
Abbreviations & Definitions
This figure shows the neck compartments used by surgeons to delineate the areas of lymph node metastases.
| Level I: | Contains the nodes of the submental and submandibular triangles, defined inferiorly by the diagastric muscles. | 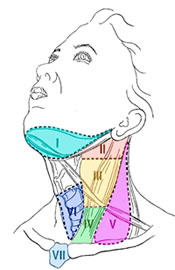 |
| Level II: | Contains the upper jugular nodes from the base of scull to hyoid bone. | |
| Level III: | Contains the middle jugular nodes from the hyoid bone to the inferior edge of the cricoid cartilage. | |
| Level IV: | Contains the low jugular nodes from the cricoid cartilage to the clavicle. | |
| Level V: | Contains the nodes of the posterior triangle that is bounded anteriorly by the sternocleidomastoid muscle and posteriorly by the trapezius. | |
| Level VI: | Contains the nodes of the anterior central compartment from the hyoid bone to the manubrium with lateral boundaries being the carotid arteries | |
| Level VII: | Contains the superior mediastinal nodes from the level of the superior edge of the manubrium to the innominate vein. | |


