WHAT IS THYROID EYE DISEASE?
Thyroid eye disease (abbreviated as TED) is an autoimmune disease that affects some people with autoimmune thyroid disease. TED is most common in people with hyperthyroidism due to Graves’ disease and rarely, may occur in patients with normal or low thyroid levels.
- About one in every three people with Graves’ disease develop eye symptoms.
- While eye symptoms can occur at any time, they usually appear within the first year of diagnosis of Graves’ disease.
- TED is usually mild and gets better on its own over time.
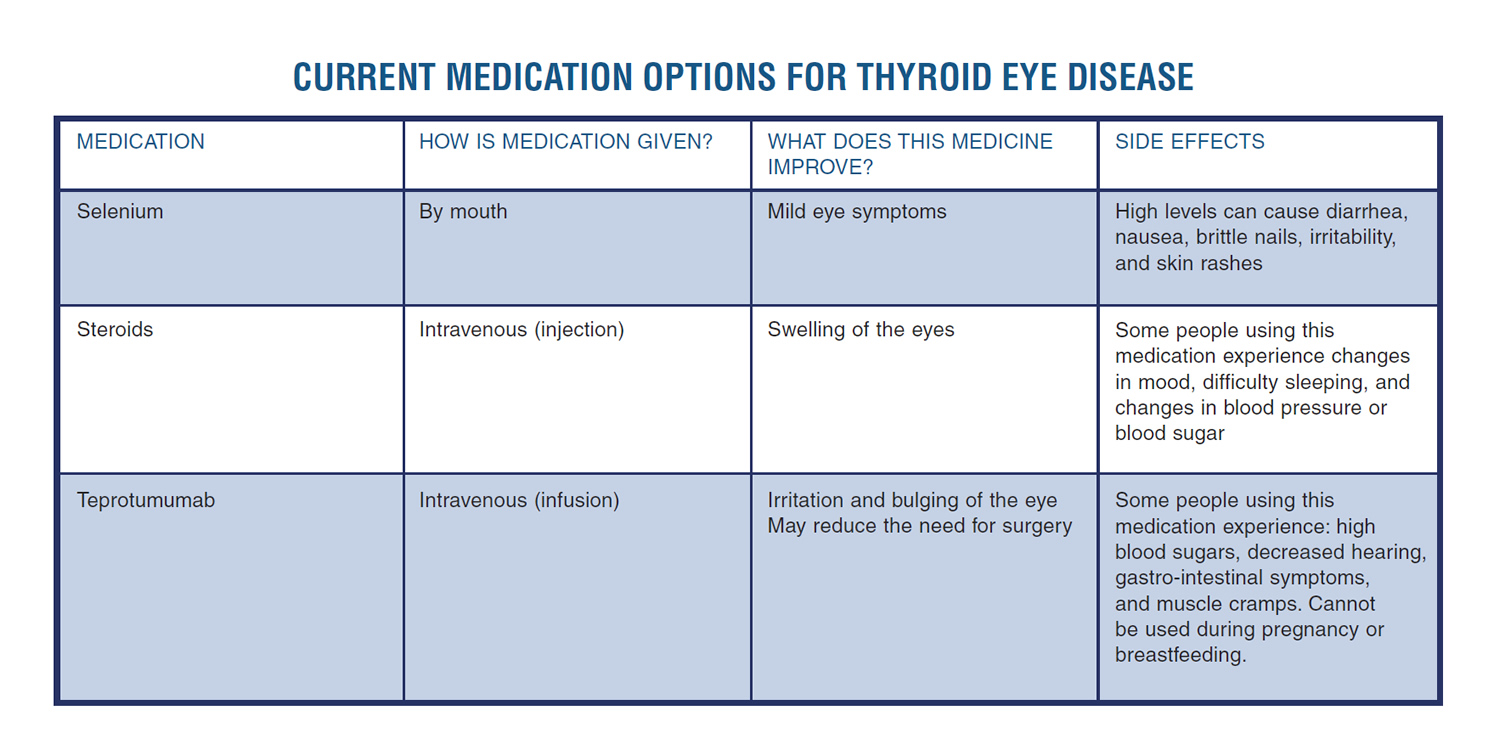
- Some cases can be quite severe and can require medications or surgery.
Symptoms of thyroid eye disease include:
- Feeling of grittiness in your eyes (like “sand in your eyes”) and sensitivity to light
- Pain behind your eyes or with eye movement
- Redness of the eyes due to swelling/irritation of the thin coating (conjunctiva) that covers the white part of the eyes
- Dry eyes
- Extra tearing of the eyes
- Puffy or red eyelids
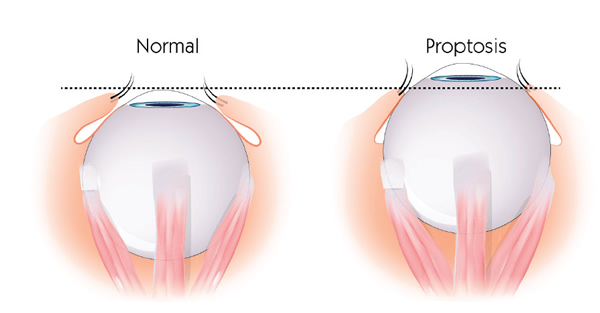
- Forward bulging of your eyes (proptosis)
- Seeing double (Double vision)
If you notice any of these symptoms of more serious eye disease, contact your doctor immediately.
- If your eyelids cannot close fully due to TED, the outer surface of your eyeball can be injured.
- If you notice a change in how you see colors
- If parts of your field of vision are lost (this can happen if your optic nerve is compressed.)