There is no single treatment that is best for all patients with hyperthyroidism. The treatment that you and your doctor decide on will take into account factors such as your age, your symptoms, and other medical problems (ex. heart disease). It also depends on the cause of hyperthyroidism and how abnormal the tests are.
See information about Understanding Thyroid Function Tests. You should consult with your endocrinologist to determine your treatment plan.
Understanding Thyroid Function Tests
|
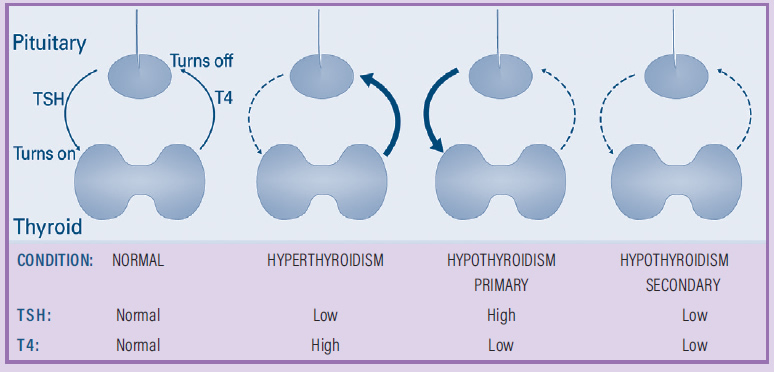
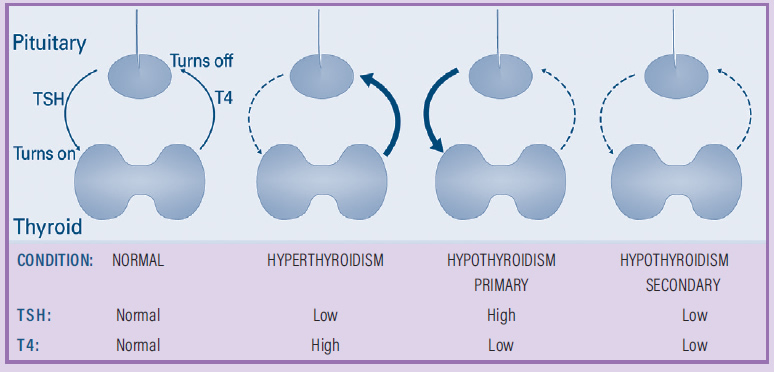
Thyroid function tests are blood tests that allow your doctors to understand the signals to and from the thyroid gland. The pituitary is the master regulator for many of the hormones in the body. The pituitary releases thyroid stimulating hormone (TSH) to tell the thyroid gland what to do.
- A higher TSH level means that your pituitary gland wants your thyroid gland to make more thyroid hormone.
- A lower TSH level means your pituitary gland wants your thyroid gland to make less thyroid hormone.
- Sometimes, the TSH level is close to zero, and that means there is too much thyroid hormone in your body and your pituitary is trying to stop your thyroid gland from making more thyroid hormone. However, the conditions that cause hyperthyroidism do not respond to (listen to) the TSH signal and continue to make (keep making) too much thyroid hormone.
The thyroid gland makes two thyroid hormones: thyroxine (T4) and triiodothyronine (T3).
- Normally, the thyroid gland makes mainly T4 and only a small amount of T3. T4 is changed into T3 in other places in the body.
- In hyperthyroidism, the thyroid gland usually makes extra amounts of both T4 and T3 but in some cases it only makes too much T3.
|
There are several treatments that may be recommended:
1. BETA BLOCKERS:
Beta blockers are medications that help control your symptoms such as rapid heart rate, shakiness, and nervousness until your thyroid hormone levels have improved.
- They do not change thyroid hormone levels.
- Beta blockers can be started even before you know the cause of hyperthyroidism.
- They can be used along with another treatment (see below) to control your symptoms until your thyroid hormone blood levels come down.
- Examples of these medications may be propranolol, atenolol, and metoprolol.
2. ANTITHYROID DRUGS (ATD) – METHIMAZOLE (MMI) AND PROPYLTHIOURACIL (PTU):
ATDs work by decreasing the ability of your thyroid cells to make new thyroid hormones. These drugs are not effective for thyroiditis.
- They do not cause a permanent reduction in your thyroid hormone levels but keep the levels controlled while you are taking the medication. The dose of the ATD needs to be adjusted to keep your thyroid levels in the normal range.
- ATDs can be used long-term or can be used shortterm as a bridge to one of the permanent options described below.
- In some patients, Graves’ disease gets better while taking ATDs and these drugs can be stopped.
- Since toxic nodules do not go into remission from treatment with ATDs, the ATD must be continued to control hyperthyroidism.
- MMI is usually preferred over PTU because of less side effects, with certain exceptions such as pregnancy.
- Extra precautions are needed if these medications are used in pregnancy. If you find out you are pregnant, you should contact your doctor immediately. A change in medications is sometimes necessary.
- Here are the important side effects to know about:
- Red skin rash or hives – if this happens, you should contact your doctor immediately to decide on the next steps.
- Liver injury (rare) – if you notice yellowing of your eyes or skin, itching, or dark urine you should contact your doctor immediately as you may need to stop the medication.
- Low white blood cells (rare) – this is called agranulocytosis and can become a life-threatening problem.
- If you develop a fever or severe sore throat while taking this medication, you should seek medical care immediately to get a complete blood count (CBC) checked and not take any more doses of the medication until you are cleared by your doctor to restart the medication.
- It is very important to discuss any side effects with the clinician who is treating your hyperthyroidism.
3. RADIOACTIVE IODINE (RAI):
Radioactive iodine works by destroying the thyroid cells that are making thyroid hormones. This treatment works for Graves’ disease and toxic nodules but is not effective in thyroiditis.
- The RAI treatment is based on how the thyroid gland uses iodine to make thyroid hormone:
- Iodine is the main ingredient the thyroid uses to make thyroid hormones. Thyroid cells pull iodine from the blood into the inside of the cell. Overactive thyroid cells pull in more iodine than usual.
- Therefore, when a small dose of radioactive iodine is given as a tablet or liquid, it travels to the thyroid gland and is taken into the overactive thyroid cells.
- Over several weeks to months, the radiation attached to the iodine destroys the overactive thyroid cells. The gland or nodules usually shrink in size and the thyroid hormone levels drop either back to normal or to low levels (hypothyroidism).
- If you have Graves’ disease, your doctor will choose a dose of RAI to try to shrink enough of the thyroid gland to cause permanent hypothyroidism.
- If you have a toxic nodule, the goal is to only destroy the overactive nodule, but leave the rest of the thyroid functioning normally. However, some patients will still develop hypothyroidism.
- After treatment, your thyroid blood tests are closely monitored every 1-3 months.
- Once you develop hypothyroidism, you will need to take thyroid hormone replacement every day for the rest of your life (see Hypothyroidism brochure).
- Almost all patients are treated with a single dose of radioactive iodine, but about 10% of people may need a second dose.
- Safety. Radioactive iodine treatment is very safe and has been used to treat hyperthyroidism for many decades.
- Radioactive iodine leaves the body through different body fluids like urine and saliva. Therefore, you will be given precautions for activities like not sharing silverware, cleaning up in the bathroom, and avoiding (or reducing) contact with others, particularly pregnant women and young children (see Radioactive Iodine brochure).
- Radioactive iodine should not be used if you are pregnant or breastfeeding.
- Treatment with radioactive iodine can make Thyroid Eye Disease (TED) get worse. If you have TED, your doctor can help you decide about RAI treatment.
4. SURGERY:
Hyperthyroidism can be cured by surgical removal of the overactive thyroid gland or nodules.
- The entire thyroid is removed for Graves’ disease.
- Only half of the thyroid may be removed in certain toxic nodules.
Hyperthyroidism must be controlled prior to surgery with ATDs, beta blockers, or other medications. If you have Graves’ disease you may be asked to take a special iodine liquid for 7-10 days before surgery.
Thyroid surgery is generally safe in the hands of an experienced thyroid surgeon. It is important to choose an experienced surgeon who performs thyroid surgeries often to decrease the risk of complications.
- Complications may include:
- damage to your parathyroid glands. These glands are located next to the thyroid gland and control your body’s calcium levels. If your parathyroid glands are damaged it can cause problems with low calcium levels.
- damage to the nerves that control your vocal cords, causing you to have a hoarse voice.
If your entire thyroid gland is removed, you will become hypothyroid since your body can no longer make thyroid hormone. Thyroid levels are restored to normal by treatment with a daily thyroid hormone replacement (see hypothyroidism brochure). If only part of your thyroid is removed, you will need to follow with your doctor to determine if you need thyroid hormone replacement after surgery.