WHAT IS MULTIPLE ENDOCRINE NEOPLASIA TYPE 2 (MEN 2)?
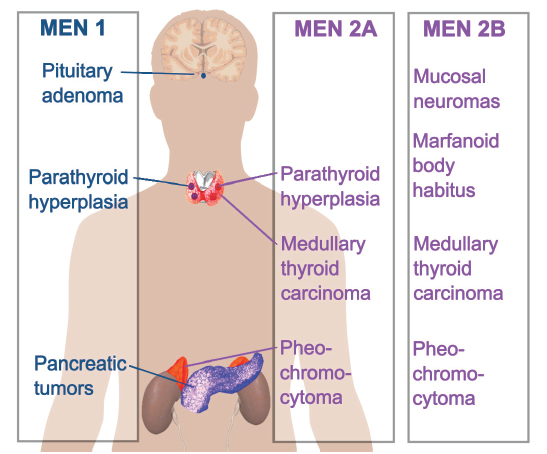
MEN 2 (Multiple Endocrine Neoplasia Syndrome type 2) is a group of diseases including a type of thyroid cancer called Medullary Thyroid Cancer (MTC). MEN2 is due to a change (mutation) in a gene called RET. This gene mutation can be found with a blood test for genetic testing. If you have changes in this gene, you [and your family members] are at a higher risk of getting MTC and other tumors.
There are two types of MEN2: MEN 2A and MEN 2B. It is important for your doctor to know the exact change you have in the RET gene to know your risk for getting the diseases in MEN2.
If you are diagnosed with either form of MEN2, you will need life-long monitoring by an endocrinologist. Depending on the diseases identified as part of the MEN2 syndrome, you may need a team of doctors to monitor for these disorders.
MEN 1 is a different condition. It is not associated with thyroid cancer.
What are the Symptoms of MEN2?
- IF YOU HAVE MEN 2A, YOU MAY HAVE:
- A form of thyroid cancer called medullary thyroid cancer (MTC)
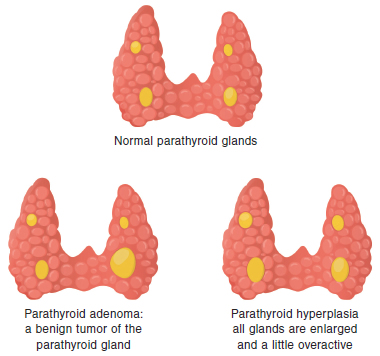
- Benign (not cancer) growth of the parathyroid glands (primary hyperparathyroidism)
- Adrenal tumors called pheochromocytoma (PHEO)
- A skin disease called cutaneous lichen amyloidosis (CLA)
- A disease of the large intestine called Hirschsprung disease (HD)
- IF YOU HAVE MEN 2B, YOU MAY HAVE:
- Medullary thyroid cancer (MTC) at an early age, even as a child
- A 50% chance of getting pheochromocytoma (PHEO)
- Other symptoms, including:
- Long arms
- High arch of your foot
- Swelling of your nerve cells (neuromas or “ganglioneuromatosis”) in the lining of your eyes, mouth, and large intestine. This can cause:
- Your eyelids to turn out
- Difficulty making tears
- Your lips appear swollen and lumpy
- Your tongue may be thick and lumpy
- Your large intestine may not work normally causing constipation or diarrhea